Why Do Umbilical Cord Blood Transplants (UCBT) Are a Better Choice?
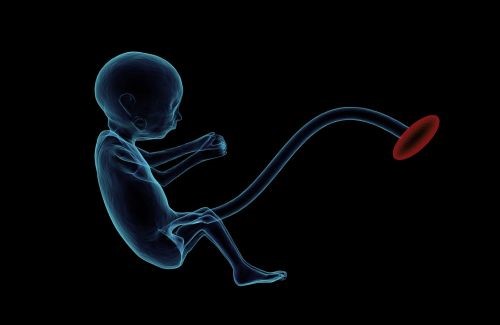
Umbilical Cord Blood Banking
Approximately 700,000 umbilical cord blood (UCB) units have been donated for the use of the public. Given the connection between the dose of cell and engraftment, many centers are selecting larger units (based on total nucleated cell count or CD34+ dose) for transplantation, even for pediatric patients. There are presently more than 100 UCB banks that are collecting units for the use of the public in North America, Europe, Asia, South America, Australia, and the Middle East. In the United States, federal laws need that a UCB must either be licensed by the Food and Drug Administration (FDA) or used under an Investigational New Drug (IND) protocol.
Private or family UCB banks gather units for family use; approximated 4 million units have been stored to be used privately. It is an innovative procedure to use private donations to fund the side of public banking, and families could choose to have privately stored UCB units present for patients who are in need.
Major Challenges in Umbilical Cord Blood Banking
- Regulatory issues, such as licensure, have extended the expense to bank UCB units.
- Less than 1 in 10 stored UCB units are being used for transplantation, also increasing the expenses.
- Some obstetrical practices, such as delayed clamping of the cord, might affect the volume and dose of cells being collected.
Future Directions in Umbilical Cord Blood Banking
Umbilical cord blood banking has adjusted to economic challenges by carefully selecting units to human leukocyte antigen (HLA) type, freeze, and store. Many banks have increased the minimum cell dose to 125 or 150 × 107 nucleated cells before processing units of UCB. In addition, the use of automated practices of freezing is more common. Innovative ways to use public and private funds to support initiatives of UCB are ongoing. Newer ways to defrost UCB cells at the transplant center, using a dilution and no‐wash method, might increase cell recovery.
Cord Blood Transplant for Hematologic Diseases
Umbilical cord blood transplant (UCBT) is a possibly healing therapy for patients with lymphoma, myeloma, leukemia, myeloproliferative disorders, genetic diseases, and disorders of metabolism. UCB is especially crucial for patients of non‐Western European ancestry because these patients have a hard time finding a matched volunteer donor in the registry of the donor. The use of double cord transplants of blood and reduced regimens of intensity in adults has led to increased use in older patients and reduced mortality related to transplants.
Major Challenges in Cord Blood Transplant for Hematologic Diseases
- Engraftment and immune reconstitution are delayed which leads to an increased risk of infection.
- The price of acquisition of two cord grafts of blood (for double cord transplant of blood in adults) can be $80,000, along with the cost of the admission for transplant and instant post‐transplant care.
- The relapse of the main disease remains the major reason for death for patients post‐transplant.
Future Trends in Cord Blood Transplant for Hematologic Diseases
There are many techniques that are under examination to enhance immune engraftment and reconstitution. Expansion trials involve efforts with mesenchymal progenitor expansion of cells which showed neutrophil engraftment of 15 days, enhanced from a historical control of 24 days. Using the notch ligand Delta 1, Delaney and colleagues enhanced neutrophil engraftment to 16 days. This work has now been outstretched to use an “off‐the‐shelf” non‐HLA‐matched expanded product of UCB, and a phase II study is ongoing (NCT01690520). The use of chelation of copper led to the evolution of the NiCord product, which showed an overall survival of one‐year of 82% and 11 days to neutrophil engraftment in a study of phase I. The product lately obtained advance designation from the FDA, and a phase III registration trial comparing expanded versus unexpanded UCB is in progress (NCT02730299). While expansion studies are favorable, the studies have been restricted by the small size of the sample and complex technology that might be tough to export to other centers.




